

Where Are We Today?
Age by itself is not a determining factor in medication nonadherence. Rather, there are many factors that may combine to render older persons less able to adhere to their medication regimens. However, there is evidence to suggest that with the proper motivation, education, and support, older persons can overcome many barriers to medication adherence (US Department of Health and Human Services, 1990).
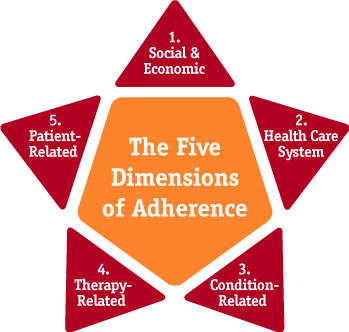
Adherence is a multidimensional phenomenon determined by the interplay of five sets of factors, termed "dimensions" by the World Health Organization (Figure 2):
- Social/economic factors
- Provider-patient/health care system factors
- Condition-related factors
- Therapy-related factors
- Patient-related factors
Patient-related factors are just one determinant of adherence behavior (World Health Organization, 2003). The common belief that a person is solely responsible for taking their medications often reflects a misunderstanding of how other factors affect people's medication-taking behavior and their capacity to adhere to treatment regimens. Factors associated with each dimension are listed in Table 2.
It is clear that adherence is a complex behavioral process strongly influenced by the environments in which people live, health care providers practice, and health care systems deliver care. Adherence is related to people's knowledge and beliefs about their illness, motivation to manage it, confidence in their ability to engage in illness-management behaviors, and expectations regarding the outcome of treatment and the consequences of poor adherence (World Health Organization, 2003).
It is important to recognize that a person may have multiple risk factors for medication nonadherence. Also, factors that can influence a person's medication-taking behavior may change over time. Therefore, it is important to continually assess a person's adherence throughout the course of therapy. In addition, because there is usually no single reason for medication nonadherence, there can be no "one size fits all" approach to improving adherence.
Many of the interventions used to improve adherence focus on providing education to increase knowledge; simplifying the medication regimen (fewer drugs or fewer doses); or making it easier to remember (adherence aids, refill reminders). However, simplifying a dosage regimen is unlikely to affect a person who does not believe that taking medications is important or that the therapy will improve his or her health, and the available evidence shows that knowledge alone is not enough for creating or maintaining good adherence habits (World Health Organization, 2003).
Based on published studies, it is evident that single interventions are less successful than multiple, long-term interventions in affecting adherence. Studies have shown that the most successful interventions have some follow-up component and address the underlying reason(s) for nonadherence (Krueger et al., 2003). Comprehensive interventions should address a variety of issues, including knowledge, motivation, social support, and individualizing therapy based on a person's concerns and needs (Krueger et al., 2003; McDonald et al., 2002).
The ideal time to initiate adherence interventions is when therapy first begins. Interventions that are initiated early in the course of therapy can support older persons through a period when they are most likely to have questions or to experience side effects from therapy.
|
|
World Health Organization, 2003; Krueger et al., 2005; Osterberg and Blaschke, 2005

